This week, we’re kicking off a new chapter in our blog: Micromate™ case report.
We’re doing it because you can’t just talk the talk, you need to walk the walk, and nothing comes closer to experiencing Micromate™‘s skillset than having real cases portrayed by actual physicians that are currently using it.
For our first case report, we head out to the Ordensklinikum Linz Barmherzige Schwestern Hospital’s Department of Diagnostic and Interventional Radiology, in an intervention led by Dr. Alexander Kupferthaler.
Clinical Context
Patient’s profile: 43-year-old female, with breast cancer and colon carcinoma, and a single metastasis in liver segment VIII, histologically proven to be a secondary blastomatous lesion from breast cancer.
Reasoning for Robotic Approach
Surgical removal of the breast and colon primary tumor was the preferred treatment. The single liver metastasis was treated with a percutaneous, robotic-guided Microwave Ablation using Angio CT/MRI fusion, as the lesion was not detectable using Ultrasound or CT.
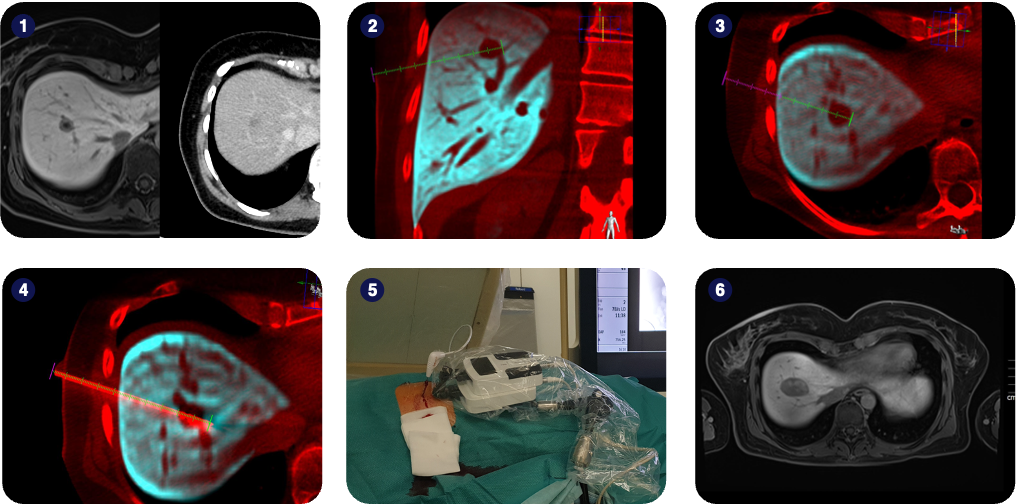
1) Pre-operative MRI and CT scan. MR clearly shows the metastasis in liver segment VIII, detectability on CT is low to none;
2-3) Coronal and transversal planes of fused AngioCT/MRI volumes with planned needle entry, path and target;
4) Microwave ablation needle positioned according to the surgical plan;
5) Clinical setup overview during the ablation step;
6) The final ablation zone as shown on follow-up MRI.
Interventional Procedure
Image fusion and planning were performed using a Philips Allura Xper FD20 angiography device and the Xper Guide planning software.
The Micromate™ device was gross-positioned near the predefined entry-point and remotely controlled for alignment to the surgical plan under fluoroscopic live imaging.
After robotic alignment, the 15G microwave needle was inserted along the predefined trajectory through the Micromate™ needle guide, again under fluoroscopic live imaging.
Ablation was then performed with 100W of power for 4 minutes, resulting in an ellipsoid-shaped ablation zone with a good safety margin.
Six months after treatment, the patient is in complete remission, showing no signs of vital tumor in the liver.
Key Takeaways
Micromate™ helped the clinical team critically increase the likelihood of reaching the liver metastasis for treatment, whose texture rendered it almost undetectable in CT and US.
Micromate™’s live-imaging capabilities made operating soft tissue such as the liver more seamless, since they allow to compensate target displacement in real-time.